How Gallup Indian Medical Center Grew a Successful HIV Program on the Navajo Nation

Source: USA Today
When Dr. Jonathan (Jon) Iralu was a medical resident at Harvard in the early 1990’s, the AIDS epidemic was at its peak, and Boston was hit hard. This experience, although challenging and full of loss, was formative for Jon, who spent nearly three decades researching and treating infectious diseases, including HIV, at Gallup Indian Medical Center.
Located on the outskirts of the Navajo Nation, Gallup Indian Medical Center (GIMC) is known for having one of the largest patient populations of all Indian Health Service (IHS) facilities. In 1994, when Jon first arrived, he began seeing patients, mostly young men, coming in with advanced HIV disease. According to Jon, at this time before anti-retroviral therapy (ART), it was not uncommon for patients to come to the clinic, receive a diagnosis, and then not survive a month.
Tragic losses motivated organization and action
In those early days, GIMC lost about 30% of their HIV+ patient population, which was as equally frustrating as it was tragic.
Out of this grief flowed the desire to better support patients. From Jon and his colleagues’ perspective, it seemed natural to create a dedicated HIV clinic and better organize the ways GIMC delivered care to HIV+ patients.
As the team began organizing their efforts, ART became available. After experiencing the loss of so many patients, Jon and his colleagues were in awe of how these new drugs allowed patients who were once terminal to turn the corner.

Source: NY Times
Building a successful HIV program
With the arrival of ART in 1996, two volunteer pharmacists stepped forward. These pharmacists regularly met with HIV+ patients prior to their primary care visits and during medication pick-ups to offer vital education, discuss medication adherence, and develop strategies for overcoming barriers to treatment.
According to Jon, community partners were also critical at this time for making the burgeoning HIV program at GIMC a success. During these early years, program staff heavily collaborated with the Navajo AIDS Network, an organization dedicated to providing home-based case management to HIV+ patients. They also ensured that patients had transportation, insurance, and other needed social supports.
The birth of HOPE
Observing the successes of this community-driven, home-based service model, Jon and his colleague, Dr Sonya Shin, worked with the late Dr. Paul Farmer, of Harvard Medical School, to implement a formalized homecare medical model on the Navajo Nation.
With an unrestricted grant from Brigham and Women’s Hospital to the federal government, GIMC was able to start Project HOPE, an initiative that is still in place today that provides directly monitored therapy to HIV+ people in their homes.
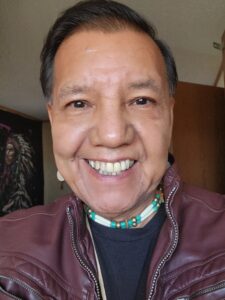
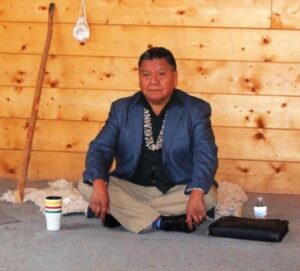
At the heart of Project HOPE (which stands for HIV Outreach and Patient Empowerment) are a group of dedicated multi-lingual HIV Technicians (HIV Techs). While visiting patients, HIV Techs check on medication adherence, provide education using flipcharts, bring medications, and check on other aspects of patients’ health. When needed, HIV Techs get in touch with a patient’s doctor of record.
According to Jon, “Project HOPE is effective at reducing barriers to treatment. The Navajo Nation, like many other Tribal Nations, is resource challenged, and because of its large size, patients are required to travel a significant distance along dirt roads to access care. For many of GIMC’s patients, this poses significant challenges. Project HOPE, though, with its home-based model, reduces the need for patients to do unnecessary and burdensome travel. It also helps patients with HIV discretely obtain treatment when desired.”
Source: NY Times
Minority AIDS Initiative funding allows for program growth
With funding provided by the Minority AIDS Initiative, Project HOPE has hired four HIV Techs – two in Gallup, NM, one in Chinle, AZ, and one in Shiprock, NM – expanding HOPE’s reach across three IHS service units. Additionally, 5 pharmacists rotate through the HIV clinic, following-up with patients by phone and providing home visits as needed. The project has also added an HIV Nurse Specialist, who provides comprehensive clinical case management.
Since the dissolution of the Navajo AIDS Network, Project HOPE has continued to collaborate with community partners, including the North Country Care (based out of Flagstaff and Winslow, AZ) and First Nations (based out of Albuquerque and Gallup, NM) who provide social case management to patients living in rural and remote places.
HIV case counts decline
Fortunately, this work, accomplished over decades with the support from a broad base of providers and community partners, has resulted in a significant decline in new cases of HIV at GIMC. According to Jon, since 2008, there has been a “marked and steady annual decline in new patient HIV diagnosis.”
Although numbers have tremendous value in telling this story of success, so too do the experiences of Project HOPE clients, some of whom have been receiving services since 1996. According to Jon “the majority of our clients now come to us via word of mouth and primary care referrals.”
This sentiment denotes the dedication and passion GIMC staff and partners have for helping hope grow and flourish on the Navajo Nation.
Learn more
To enhance your ability to screen, treat and manage patients with HIV, join the University of New Mexico’s HIV ECHO sessions. Here you will participate in didactic and case presentations, receive recommendations from peers and a multidisciplinary team of specialists, like Jon, and join a learning community of dedicated I/T/U providers committed to growing clinical capacity so every patient across Indian Country receives the care they deserve.