Destigmatizing Treatment for Community Members with Opioid Use Disorder

In January 2019 the Family Health Centers, located in Omak, Washington, started the Opioid Treatment Network (OTN), a program designed to provide high quality outpatient treatment services for individuals with opioid use disorder (OUD).
As a National Health Service Corps site that serves all community members, including members of the nearby Colville Reservation, regardless of income, the Family Health Centers staff believed they could have an impact on OUD in Omak.
In order to support patients, the OTN team director continued to build the team, eventually hiring two committed recovery coaches, one experienced peer specialist, and two enthusiastic nurse care managers, all of whom had specialized training on treating individuals with substance use disorders. However, despite the OTN’s high hopes and competent staff, initially patients did not seek care.
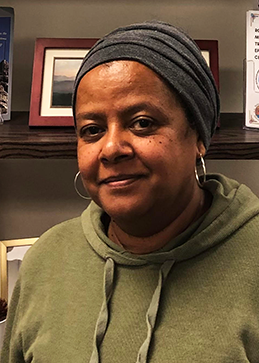
When Briana Pardo, a Colville Tribal member, began working for the OTN as a Care Navigator in April 2019, there were only five patients in the program and many widespread misconceptions existed across the community about OTN’s services. However, after extensive community outreach, two years later many things have changed. As of April 2021, OTN’s active patient cases has grown to over 150, and they are now collaborating with several community organizations to provide their patients with valuable wrap around medical and social services.
To explain the growth in patients accessing care, Briana, who is now the Nurse Care Manager Lead, began by sharing the history of OUD treatment in Omak. She explained that prior to the OTN’s inception, the health center provided buprenorphine, a medication that helps curb craving for some with OUD. Once OTN opened though, they expanded the services available in the community. They also began collaborating with other health and service providers in the area.
Part of OTN’s success, according to Briana, stems from the program’s ability to provide a broad spectrum of services to meet the needs of patients through partnerships. The OTN collaborates with OK COPE (Okanogan Community Overdose Prevention Education), to offer naloxone training and kits, information about accessing clean syringes, fentanyl test strips, and information about treatment services available. All OTN staff carry naloxone so they can assist in an overdose, but also to be able to offer naloxone and naloxone trainings whenever the need arises. Additionally OTN works with the Okanogan Behavioral Healthcare to ensure patients have access to individual and group behavioral health services, as well as recreational activities, such as yoga, to assist with their recovery.

Another aspect of the program Briana believes has resulted in more individuals accessing services is OTN’s team-based approach to care. OTN staff meet monthly with all of their patients’ providers to discuss treatment plans. Also, an OTN staff member meets monthly with Okanogan Behavioral Healthcare providers to review and coordinate patients’ care plans. Everyone on the OTN team and their collaborators work with patients to encourage them to stick with the program and obtain the treatment they need. They educate patients on their treatment plan, help patients schedule appointments, facilitate transportation to and from visits, attend narcotics anonymous meetings with patients, and if patients do not have insurance, they connect them with the enrollment department.
One final piece Briana attributes to OTN’s growth, is that OTN staff took steps to educate community members and providers about substance use treatment. According to Briana, “There was a large misconception in the community that there were no services to treat substance use disorder and that there was nothing people impacted by opioids could do about it. In fact, there is so much that we can do about it!” Some of this work happened through community naloxone trainings and educating family members about services available. Some of this happened through reaching out to providers, some of whom were initially hesitant. But after working with and seeing the impact of OTN, several providers felt confident prescribing MAT as a part of patients’ recovery. Today, in addition to those on the OTN team, the Family Health Centers now has over 15 medication-assisted treatment (MAT) providers.
By addressing misconceptions, forming community partnerships, increasing providers’ comfort with prescribing MAT, and treating patients with kindness and compassion, OTN has been able to provide services to hundreds of patients and connect them with needed medical and social service resources. Briana says, “Every time someone uses suboxone instead of heroin, it is a time they will live to see another day.” For Briana and her colleagues at OTN, this inspires them to continue to do the work they do and serve as many community members as possible.

To enhance your ability to screen, treat and manage patients with OUD, join one Indian Country ECHO’s Substance Use Disorder virtual clinics. Here you will participate in didactic and case presentations, receive recommendations from peers and a multidisciplinary team of specialists, and join a learning community of dedicated I/T/U providers committed to growing clinical capacity so every patient across Indian Country receives the care they deserve.