Caring for People with Substance Use Disorders Using Evidence- and Culture-based Treatments


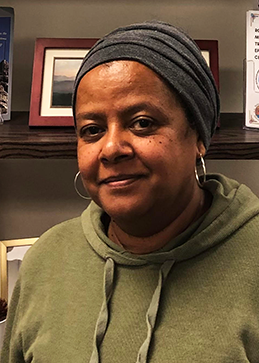
In 2016, Laura Hamilton, a Certified Substance Use Disorder Professional, began working at Shoalwater Bay Wellness Center’s Chemical Dependency Program counseling patients with substance use disorders (SUDs). Initially, the Chemical Dependency Program Manger encountered some reluctance from community members. According to Laura, “In Native Country it can take a while for people to get used to a therapist when they come in brand new.”
To address this barrier to care Laura, began extensive community outreach across Tokeland, Washington, as well as the neighboring Grays Harbor and Pacific Counties. “It’s a matter of being involved in different programs and getting my face out there … to be able to get community members to feel comfortable enough to come see me.” For example, at a new initiative called Náwsanti, which means “first foods,” Shoalwater staff, including Nutritionist Pam Drake, and several tribal members, provided 60 community members a traditional meal that included fish on a stick, oysters cooked in the shell, nettle soup, traditional salads, and more. Participants received blueberry and sloe bushes to grow at home, and a cultural knowledge bearer presented on the role of food in our overall wellness, including food’s potential to help those healing from substance use disorders. Also Laura began advertising the Chemical Dependency Program’s outpatient mental health and other services available in phone books, clinical referral lists, and in other community resources.
According to Laura, these efforts paid off. In the four years since she joined, the program has doubled the number of active clients served. In addition to individual therapy, which incorporates teachings from the Red Road to Wellbriety, Shoalwater’s Chemical Dependency Program offers two group sessions weekly focused on supporting patients in maintaining their recovery.

The program also has recently started providing medication-assisted treatment (MAT), using vivitrol, a medication that blocks the effects of opioids. While they are not currently offering suboxone, the program hosts a monthly group for patients taking suboxone as part of their recovery.
To prevent death from opioid overdose, Chemical Dependency Program staff have also put a heavy emphasis on distributing and training community members and clinic staff on the use of Naloxone. Laura and other staff outreached to neighboring communities on the use of Naloxone, and trained local police, EMS workers, and other tribal social service providers on its use.
According to Laura “there were so many things that were provided for the community that it is hard to list everything. All of this could not have been completed without getting the community input on what they [the community] felt they wanted.” And her efforts are bearing fruit. Regarding this she said “I am fortunate that many individuals in active recovery stay in touch with me and let me know how they are doing. This is a gift that motivates me to continue doing this important work.”
To enhance your ability to screen, treat, and manage patients with substance use disorders, join Indian Country ECHO’s SUD virtual clinics. Here you will participate in didactic and case presentations, receive recommendations from peers and a multidisciplinary team of specialists, and join a learning community of dedicated I/T/U providers committed to growing clinical capacity so that every patient across Indian Country receives the care they deserve.